If you or a loved one has diabetes, then you know how difficult managing the condition can be. Diabetes can affect nearly every part of the body, even the parts you wouldn’t normally associate with diabetes, such as the eyes.
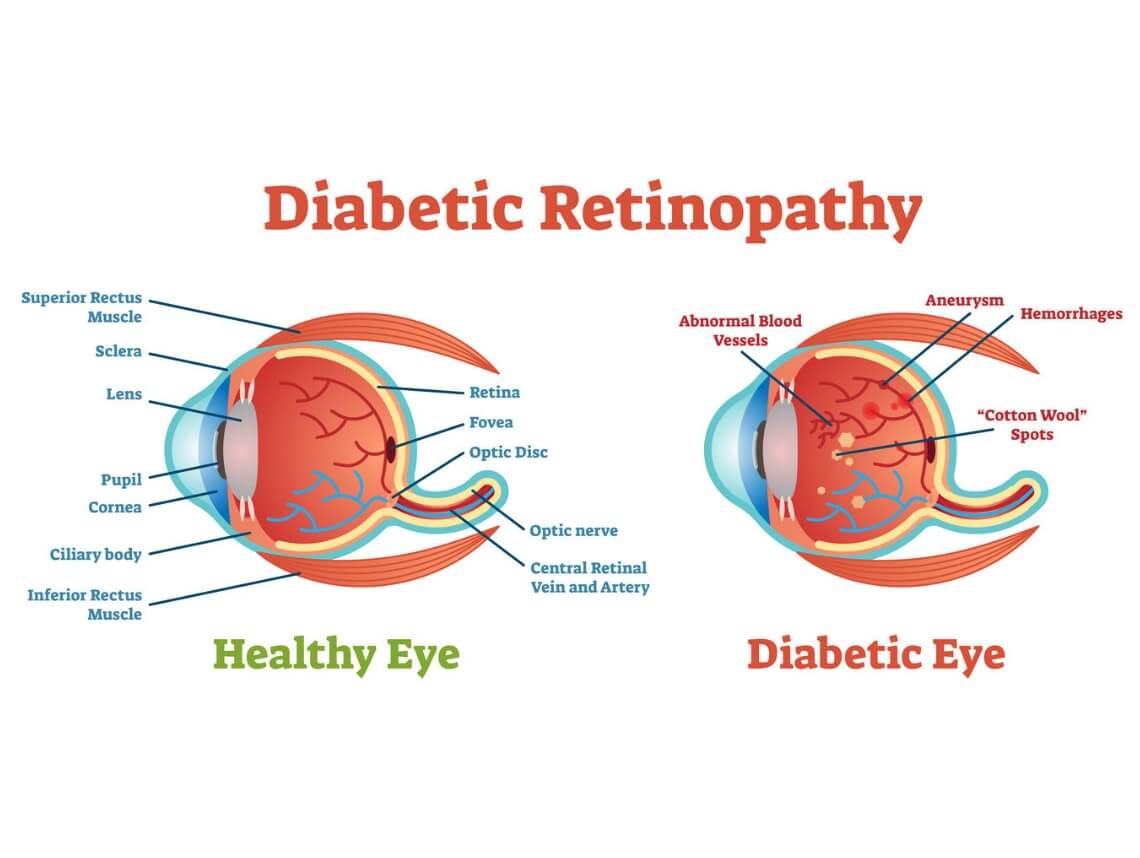
For those with diabetes, a condition known as diabetic retinopathy can be a big concern as it affects vision. The complication damages the blood vessels of the retina’s light-sensitive tissue, potentially causing blindness. The condition can develop in anyone who has type 1 or type 2 diabetes, but the longer one has diabetes and the less controlled the blood sugar, the more likely they are to develop eye complications.
If you have diabetes, our resources are here to help you protect your vision and improve your quality of life if you’re living with a diabetic retinopathy-related impairment.
Learn the symptoms, causes, diabetic retinopathy stages, treatment, and more here.
Diabetic Retinopathy Symptoms
With diabetic retinopathy, the initial stages are typically asymptomatic. When symptoms are present, they include:
- Floaters (spots or dark strings in vision)
- Distortion and blurred vision
- Fluctuating vision
- Impaired color vision
- Dark areas in vision
- Vision loss
Diabetic Retinopathy Causes
Diabetic retinopathy occurs when the tiny blood vessels that nourish the retina are blocked. This occurs when there is too much sugar in the blood over a period of time. As a result, the eye may attempt to grow new blood vessels, but many times, the new blood vessels don’t grow properly and start to leak.
Diabetic Retinopathy Stages
There are two diabetic retinopathy stages: early diabetic retinopathy and advanced diabetic retinopathy.
Early diabetic retinopathy
The first diabetic retinopathy stage is known as early diabetic retinopathy or nonproliferative diabetic retinopathy (NPDR) and is classified by weakened blood vessels in the walls of the retina. NPDR also causes tiny bulges to protrude from the vessel walls of the smaller vessels, which can cause fluid leakage in the retina. As this progresses, the nerve fibers in the retina may begin to swell and require treatment.
Advanced diabetic retinopathy
The second stage is known as advanced diabetic retinopathy. With this type of diabetic retinopathy (proliferative diabetic retinopathy), the damaged blood vessels close which causes new, abnormal blood vessels to grow in the retina which can leak into the clear, jelly-like substance in the center of the eye. As this progresses, scar tissue can form, causing the retina to detach from the back of the eye.
Diabetic Retinopathy Risk Factors
Anyone who has diabetes can develop diabetic retinopathy, but the risk increases with these factors:
- Duration of diabetes; the longer one has had diabetes, the more likely they are to develop diabetic retinopathy
- Poor control of blood sugar level
- High blood pressure
- High cholesterol
- Tobacco use
- Being African-American, Hispanic, or Native American
- Pregnancy
Diabetic Retinopathy Complications
Complications from diabetic retinopathy can lead to serious vision problems, including:
- Glaucoma: As new blood vessels associated with diabetic retinopathy grow, the pressure in the eyes can build up – a condition known as glaucoma. Excess pressure in the eye can damage the optic nerve, resulting in vision loss.
- Retinal Detachment: Diabetic retinopathy is associated with abnormal blood vessel growth in the eyes. This abnormal growth can create scar tissue which can pull the retina away from the back of the eye.
- Vitreous Hemorrhage: Diabetic retinopathy can cause the new blood vessels to bleed into the clear, jelly-like substance that fills the center of the eye. If too much blood leaks, it can fill the vitreous cavity, resulting in blocked vision.
- Blindness: Diabetic retinopathy can eventually lead to complete vision loss.
How is diabetic retinopathy diagnosed?
Diabetic retinopathy is diagnosed with a comprehensive dilated eye exam. To perform this exam, a drop is placed in the eyes to open the pupils wide which allows the doctor to view the inside of the eyes. During the exam, the doctor will look for abnormal blood vessels, swelling in the retina, bloody and fatty deposits in the retina, new blood vessel growth, scar tissue, bleeding, retinal detachment, and other abnormalities.
The ophthalmologist or optometrist may request a Fluorescein Angiography exam or an Optical Coherence Tomography (OCT) exam. The former uses an injectable dye to pinpoint issues within the blood vessels of the eye. The latter is an imaging test that provides cross-sectional images of the retina.
Diabetic Retinopathy Treatment
Treatment depends on the type of diabetic retinopathy, as well as the severity. Depending on the type and severity, the doctor will determine if treatment should be geared to slow or stop the progression of the condition.
Early Diabetic Retinopathy
Early diabetic retinopathy may not need treatment right away. Instead, the doctor will monitor the eyes closely to establish when and if treatment is needed. They will also likely suggest ways to improve diabetes management since healthy blood sugar levels can usually slow the progression.
Advanced Diabetic Retinopathy
If you have advanced diabetic retinopathy, you will need surgical treatment. The type of treatment will depend on the specific problem(s) within the retina and may include photocoagulation, pan retinal photocoagulation, vitrectomy, or injectable medicine. Each of these treatments varies, but essentially work to remove scar tissue, abnormal blood vessels, and blood.
Diabetic Retinopathy Prevention
When it comes to preventing diabetic retinopathy, there are a few things you can do to help keep your eyes healthy.
Make sure to have regular eye exams, control blood sugar and blood pressure, and address any changes in vision right away as they may be early signs of diabetic retinopathy. If you experience a change in vision – especially sudden blurriness, haziness, or spottiness – call the doctor right away.
Contact Care Options for Kids for Home Health Care Services
The American Optometric Association recommends that individuals over the age of 60 receive annual eye exams. If you’re a family caregiver juggling duties, life at home, and a career, it’s often difficult to provide loved ones with the necessary level of care, including transportation to and from appointments.
If you or an aging loved one are considering home health care services, contact the caring staff at Care Options for Kids. Call today at (888) 592-5855.
